A Little-Known “Super Fungus” Is Spreading in the U.S. — Here’s What You Need to Know
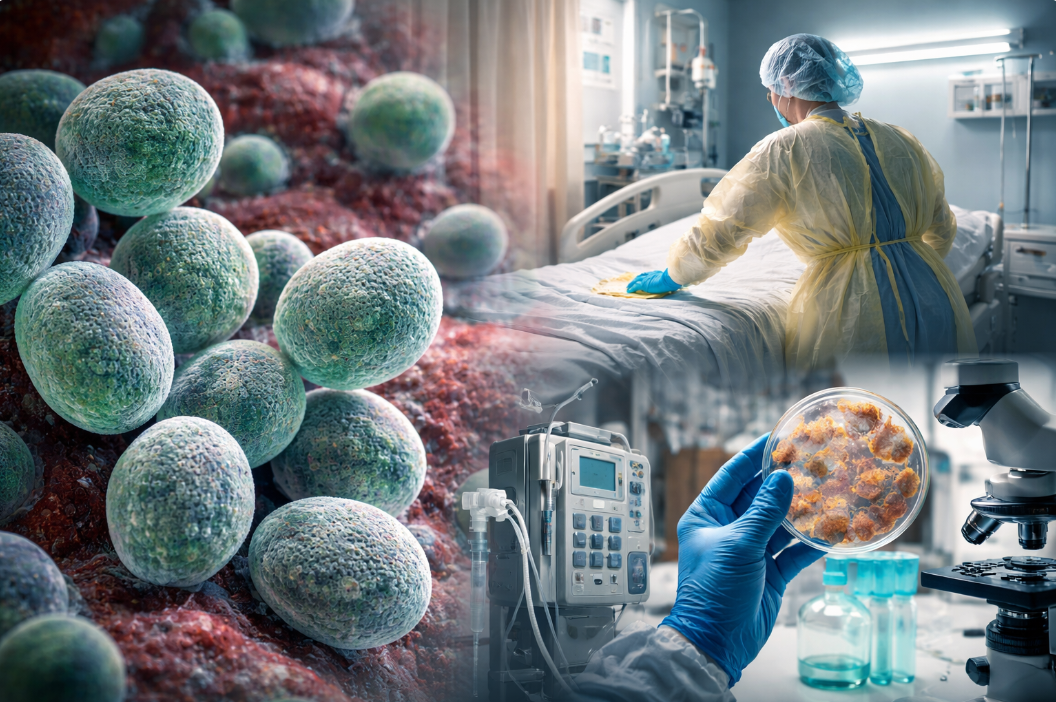
A dangerous, drug-resistant fungus most Americans have never heard of is quietly spreading across the United States, largely inside hospitals and nursing homes. Known as Candida auris, this emerging pathogen has become a growing concern for health officials because of how easily it spreads — and how difficult it can be to treat.
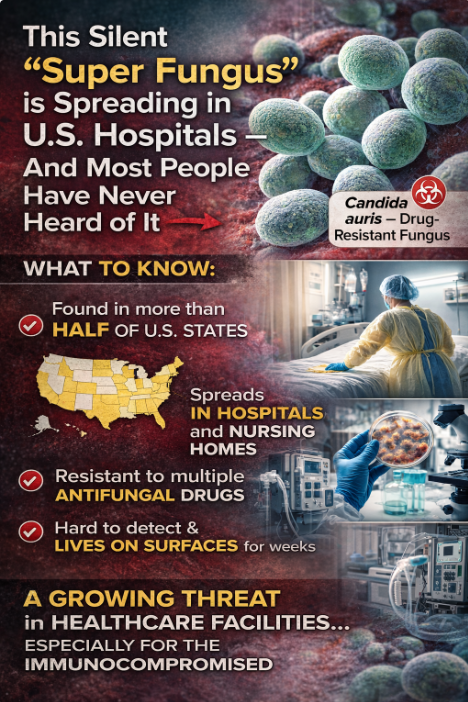
According to tracking by the Centers for Disease Control and Prevention, Candida auris has now been detected in more than half of U.S. states, with cases increasing steadily over the past several years. While it does not typically affect healthy people in everyday settings, it poses a serious risk to patients who are already ill or have weakened immune systems.
Why Candida auris Is So Dangerous
Unlike more familiar fungal infections, Candida auris can survive for weeks on surfaces such as bedrails, doorknobs, medical carts, and equipment. It spreads most often in healthcare environments through contact with contaminated surfaces or medical devices, including:
- Catheters
- Breathing tubes and ventilators
- IV lines
- Shared hospital equipment
One of the biggest challenges is that people can carry the fungus on their skin without showing symptoms, unknowingly spreading it to others in close-care environments.
Limited Treatment Options
Candida auris is especially alarming because many strains are resistant to multiple antifungal medications. Doctors often rely on a specific class of antifungals as first-line treatment, but resistance has been increasing. In rare cases, some strains have shown resistance to all major classes of antifungal drugs, leaving physicians with extremely limited options.
Health officials stress that these fully drug-resistant cases are still uncommon — but the trend is troubling.
How Widespread Is It?
The CDC has reported thousands of clinical cases nationwide in recent years, with numbers rising year over year. While exact totals for 2025 have not yet been fully released, experts say the upward trend is clear. Most confirmed infections occur in:
- Hospitals
- Long-term care facilities
- Nursing homes
Invasive infections can be serious, and in patients with underlying conditions, outcomes can be severe.
A Possible Link to Climate Change?
Some scientists believe climate change may be playing a role in the emergence of Candida auris. The theory suggests that rising global temperatures could be helping certain fungi adapt to survive at human body temperature, something that previously limited their ability to infect people. While this idea is still being studied, it has raised new concerns about future fungal threats.
What the Public Should Know
For most people, the risk remains low. Candida auris is not typically spread in the community like the flu or COVID-19. However, awareness matters — especially for those with loved ones in hospitals or nursing homes.
Health officials recommend:
- Strict infection-control practices in healthcare settings
- Proper cleaning and disinfection of medical equipment
- Early detection and screening in high-risk facilities
- Clear communication when patients are transferred between facilities
Candida auris isn’t a household name — yet — but public health experts consider it a serious and emerging threat. Its ability to resist treatment, survive on surfaces, and spread silently in healthcare settings makes it especially dangerous for vulnerable populations.
Awareness is the first step. Knowing the risk helps families, caregivers, and healthcare providers stay vigilant as scientists and doctors work to better control this growing “super fungus.”